Current Surgical Treatments:
If drug treatments have failed to control the intraocular pressure, doctors will usually recommend surgical intervention. There are three prominent methods of attack in the armamentarium of the ophthalmologist: trabeculoplasty, trabeculectomy, ciliary body manipulation, and implantable drainage devices.
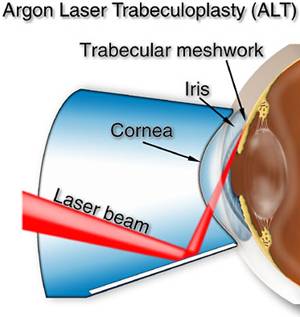
Trabeculoplasty:
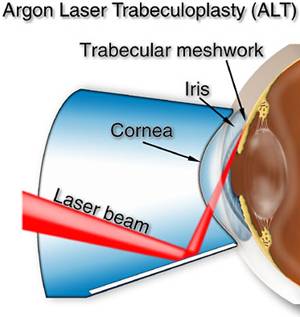
The argon laser is directed into the eye at the trabecular meshwork via a lens placed on the eye. The mechanical theory of operation in this procedure is that the electromagnetic energy carried by the 514 nm laser beam is converted to thermal energy upon contact with the trabecular meshwork. This results in heating/burning of the tissue, creating an opening and subsequent scarring within the tissue [4]. This results in tissue contraction via collagen shrinkage. This is very much the same principle applied in laser dermatology. The procedure typically involves irradiating 180 degrees of the trabecular meshwork around the circumference of the eye. This results in the scarring of a significant portion of tissue within the eye. If the procedure does not work satisfactory, the surgeon can irradiate the remaining 180 degrees in a second procedure.
One disadvantage of this technique is that scarring is induced as well as the collateral damage to surrounding tissues. Also, the procedure can only be performed twice, with significant tissue compromise. These drawbacks are functions of pulse duration and wavelength. The short wavelength results in very minimal tissue penetration while a pulse duration of 1 millisecond results in collateral damage via non specific tissue heating.
Trabeculectomy and Implantable Shunt:
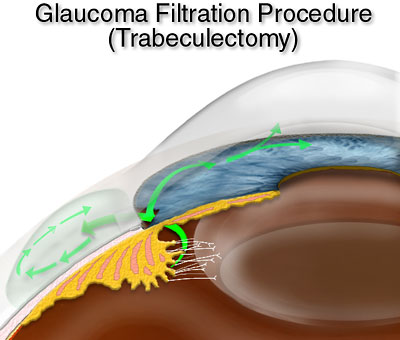
In this procedure the surgeon manually dissects a new pathway into the sclera from the anterior chamber. The aqueous humor drains into the channel within the sclera and under the conjuntiva. The AH pools here in a nonspecific way and forms a bleb, or pocket of fluid. The AH remains in the bled and is absorbed by the venous system. This procedure acts to increase the outflow facility of the system by providing a supplemental path of AH outflow. The procedure is relatively invasive when compared with trabeculoplasty and is only used when the former has failed.
A very recent advance in trabeculectomy was developed by UCI’s own Dr. Baerveldt. The innovation was a device call the Trabectome. The device physically removes portions of the trabecular meshwork via a cautery-like tip and an aspirator. See “ Ab Interno Trabeculectomy: Development of a Novel Device (TrabectomeTM) and Surgery for Open-Angle Glaucoma” in the 2006 Journal of Glaucoma for more information.
The implantable shunt works on a similar principle. But instead of surgically creating a channel into the sclera, a shunt is implanted which connects the anterior chamber to the intrascleral space via medical grade silicon tube.

I
Pictured is the Baerveldt Shunt