Aqueous Humor:
The aqueous humor is the fluid responsible for nourishing the lens and the avascular cornea, while also maintaining the intraocular pressure. The pressure is established as result of an equilibrium established between aqueous humor production and the resistance it meets on its journey out of the eye. Aqueous humor is produced by the ciliary body in the posterior chamber at a rate of roughly 2 microliter/minute. Turnover of aqueous in the eye is 1.5 – 2 hours [3]. To maintain a constant pressure within the eye the accumulation term in the mass balance for the eye must be equal to zero.
i.e. Accumulation = in – out.
Thus, the rate of secretion must be equal to the rate of outflow. The resistance to the flow is provided by the outflow structures.
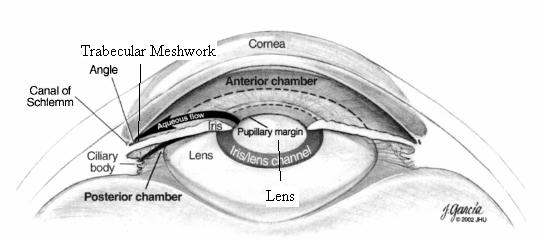
The AH is secreted by the ciliary processes at the iris root in the posterior chamber. It then flows through the iris lens gap and into the anterior chamber which is bounded by the iris and cornea. The aqueous humor circulates in the anterior chamber due to convective currents set up by temperature gradient between the cornea and iris. The fluid then flows to the angle formed by the cornea and iris. It is here the outflow structures are encountered. The AH enters the angle and passes through the trabecular meshwork, then across the inner wall of schlemm’s canal and into the canal itself, upon which the AH flows into the collector channels and into the episcleral venous system, which is at a pressure of roughly 7 mmHg.
The image shows the basic path of the aqueous humor.
x
Resistance to Flow and IOP
Now that we know the path the AH takes on its way out, we can surmise where the resistance to outflow arises. This will subsequently give insight into how one may treat elevated pressure through surgical means. The first structure encountered is the trabecular meshwork.
The trabecular meshwork is a porous zone of pores ranging from 2 to 75 microns across [1]. It is the first outflow structure encountered by the aqueous humor. However, it is thought that this region does not account for the bulk of the resistance met by the AH. McEwen (1958) used Poiseuille’s law to show that a single pore 100 mm long (the thickness of the trabecular meshwork in the flow-wise direction) and 20 mm in diameter could carry the entire aqueous humor flow (2 ml/min) with a pressure drop of 5 mmHg, and thus concluded that there was negligible flow resistance in this region [1]. This result, however, is not ubiquitously accepted as some efficacious treatments do indeed target the trabecular meshwork and succeed in lowering IOP. This illustrates one of the prevailing questions in glaucoma treatment. Where exactly does the pressure rise originate? Analytically, the trabecular meshwork should not contribute much to resistance, but observed results tell a different story.
After passing through the trabecular meshwork the aqueous humor encounters the inner wall of schlemm’s canal. It is thought that much of the resistance met by AH is originated in this tissue. Here the AH must pass a nearly solid barrier of cells which compose the canal wall. It is thought that giant vacuoles form and transport the AH across the cell lining. However, there is debate as to whether or not these are artifacts in the scanning electron micrographs used is the study. It is, however, generally accepted that the schlemm’s canal wall and juxtacanalicular tissue provide considerable resistance. Once in the canal, the AH faces essentially unimpeded flow due to the large vessel dimensions (190-370 micron diameter) as it makes its way into collector channels and ultimately the episcleral venous system.
It should be noted that the primary facets of resistance are the trabecular meshwork and schlemm’s canal. As such, any surgical procedure aimed at reducing IOP (without an implant) should target these regions.
As mentioned before the flow out of the eye is equal to the secretion rate. A simple relation can be derived to describe the role of resistance, flowrate, and pressure within the eye. It is as follows:
Q = ΔP/R.
‘Q’ is defined as the flowrate, which is constant. It is roughly 2 microliter/minute. ‘ΔP’ is the pressure difference between the anterior chamber and the episcleral venous system. It is typically 8-13 mmHg. ‘R’ is the resistance of the system to the flow. In this case, the resistance is provided by the TM and SC. Given this relation, it is easy to see that if the resistance decreases the pressure term must also decrease since the flowrate is constant. This is precisely the idea behind surgical intervention.
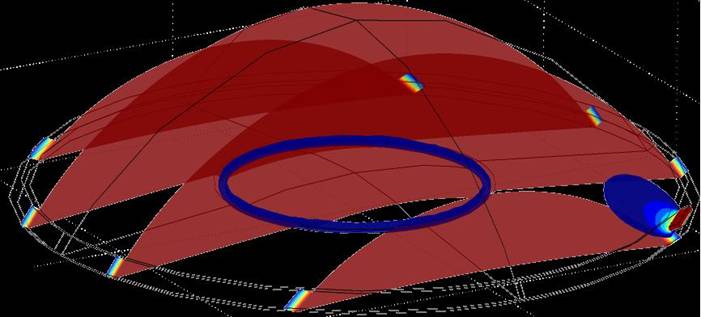
The image shows the anterior chamber and the trabecular meshwork/schlemm’s canal along with a modeled surgical channel. There is an obvious increase in flowrate across the channel, in addition to a pressure drop. The image is the result of a CFD simulation in COMSOL Multiphysics.