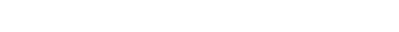
Figure 3. Percentage breakdown of deaths from cardiovascular disease (2004).
CAD: Overview
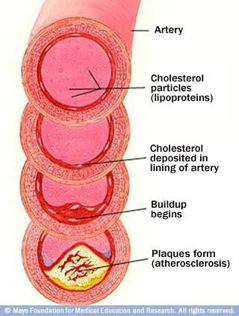
Coronary Artery Disease occurs when the coronary arteries (the arteries that supply blood to the heart muscle) become hardened and narrowed. The coronary arteries harden and narrow because of the buildup of plaque, which is composed of fatty substances, cholesterol, cellular waste products, calcium, and fibrin. The process in which the artery hardens and narrows is called Atherosclerosis, which is a type of Arteriosclerosis (general hardening of the blood vessel). In 2004, CAD has contributed to over 50% of the cases of cardiovascular disease, whereas other types of CVD made up a small percentage (Figure 3, Shuman). This is equivalent to an estimated value of 400,000 to 800,000 deaths due to CAD alone. With childhood obesity at an all-time high, the incidence of CAD may significantly increase and develop into an even deadlier disease.
There are six different coronary arteries located near and on the heart (Figure 4). The aorta is the largest of the six, while the rest are similar in size. The smaller coronary arteries are more susceptible to atherosclerosis due to their size. The size of the arteries directly influence the blood flow, flow velocity, and other parameters that may influence the development of atherosclerosis.
Coronary Artery Physiology
The coronary artery is composed of three general layers: tunica intima, tunica media, and tunica adventitia. Starting from the innermost layer, the intima is mainly composed of a monolayer of endothelial cells that lines the lumen of the artery. Endothelial cells are significant because they provide the thrombosis-resistance and produce relaxation (nitric oxide) and vasoconstricting factors (endothelin) that affect the medial layer. The next layer is the internal elastic lamina, which is essentially a sheet of elastin fibers to provide resistance to permanent deformation during vasorelaxation or constriction. The media is composed of smooth muscle cells and elastic/

Figure 4. The coronary arteries of the heart.
Causes of CAD
Through numerous years of research, the following factors are responsible for causing CAD:
* High blood cholesterol (especially LDL or "bad" cholesterol over 100 mg/dL)
* Cigarette smoking and exposure to tobacco smoke
* High blood pressure
* Diabetes mellitus
* Obesity
* Physical inactivity (Shuman)
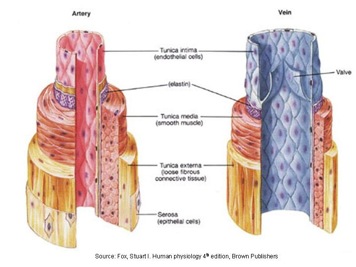
collagen tissues. The smooth muscle cells in the medial layer provide the ability to contract or relax with the factors produced by the endothelial cells, and also control the deposition of collagen and elastin. The next layer is the external elastic lamina, which has the same function as the internal elastic lamina. The final layer is the tunica adventitia, which is mostly composed of loose connective tissues such as collagen type 1. This layer provides mechanical support for the artery during relaxation or in cases of high pressure.
Figure 5. Layers of Artery & Vein.
Atherosclerosis: Theories of Genesis
There have been numerous theories in the development of atherosclerotic plaques since its discovery. The first theory was generated in 1851 by Rokitansky, whom suggested that atherosclerosis began in the intimal layer with deposition with thrombus and its organization by the infiltration of fibroblasts into the intimal layer and secondary lipid deposition. The second theory was presented by Virchow in 1856, which proposed the idea that atherosclerosis began with lipid transudation into the arterial wall and its interaction with cellular and extracellular elements, resulting with intimal proliferation. The third theory was proposed by Ross, which proposed the idea that injury to the endothelium made it susceptible to the accumulation of lipids and the development of thrombus.
The current theory that is accepted is the response-to-vascular injury theory, which is similar to Ross’s theory. The effect of vascular injury can be classified by three particular types: Type 1, 2, and 3. Type 1 injury involves changes in the endothelium with minimal structural changes such as increased lipoprotein permeability). Type 2 injury involves a disruption to the endothelium, but with minimal thrombosis. Type 3 injury involves damage to the medial layer, which can instigate severe thrombosis. Paired with various systemic risk factors such as cigarette smoking, hyperglycemia, etc, these types of injuries may cause local disturbances to the blood flow at bifurcations or angled sections of the artery, which can insinuate the series of events that lead to the development of atherosclerosis (Singh).
Atherogenesis
Once the call for an inflammatory response is set, monocytes flowing through the blood stream enter the arterial wall along with platelets adhering to the site of injury. The monocytes then differentiate into macrophages, which soak up the oxidized LDL (low density lipoprotein) particles in cholesterol, turning macrophages into large foam cells. Cholesterol plays an important role here, especially LDL and HDL (high density lipoprotein) particles. The steps where the LDL particles attract, invade, and stimulate the macrophages occur when the cholesterol is released from the LDL particles and becomes oxidized. HDL particles have the opposite function, which is to remove the oxidized cholesterol from tissues and deliver them to the liver. Therefore, if there are insufficient HDL particles in the blood stream, there is an increased risk of macrophages taking in the LDL particles. These foam cells eventually die off, which triggers a continuous cycle of events for the inflammatory response.
Diagnostic Examinations
The first test that is usually conducted is the resting electrocardiogram (EKG), which records the electrical activity of the heart. The EKG can print out a series of curves that can show signs of ischemia (oxygen starvation) or heart attacks by looking at certain peak heights and patterns. Another useful test is a stress test, which involves exercise on a treadmill. This test is useful as a screening test for patients with moderate chances of having significant CAD, yet has a regular EKG reading. The accuracy of this test method ranges between 60-70%.
If these test do not yield any results for diagnosis, adding a nuclear agent intravenously during the stress test can allow for much better imaging of the blood flow through the coronary arteries. These nuclear agents usually have a very short half-life, allowing for a very short time period for imaging. Usually, a region of the heart with significantly reduced blood flow during exercise is a good indicator of the existence of partial arterial stenosis.
The most accurate, yet invasive test for determining CAD is cardiac catheterization with angiography. In this examination, catheters are usually fed and inserted into an artery (usually the femoral artery) and eventually led to two main arteries (left and right coronary arteries). The catheter is routed through the arterial system with the assistance of an X-ray machine. Once the catheter is in place, an iodine-based contrast dye is injected into the arteries while an X-ray video is captured. In certain special cases, exercise is done simultaneously to determine the degree of narrowing. Although this test is the most invasive of the current available test, it has the highest certainty with respect to accuracy (MedicineNet: CABG). Once the existence of CAD is confirmed, there are numerous options to treat CAD such as nitroglycerin, beta and calcium blocking agents, and heparin treatments. However, the most successful treatment of CAD is a procedure called Coronary Artery Bypass Surgery.

Simultaneously, the smooth muscle cells (SMCs) in the medial layer undergo intimal hyperplasia, which is when SMCs proliferate and migrate into the intima due to the cytokine expression by the damaged endothelial cells and the encouragement by the foam cells and platelets. Eventually, the medial layer gets replaced by extra collagen deposited by the SMCs, while the SMCs themselves gradually transform into foam cells. This cycle ultimately results with a fibrous encapsulation around the fatty streaks and the intima. The fatty streaks produce enzymes that gradually enlarge the artery; however, if the lumen of the artery is not large enough to accommodate the atheroma while providing sufficient blood flow, ischemia may set in. Furthermore, if the enlargement of the artery is beyond proportion to the atheroma thickness, an aneurysm may form (Singh).
Figure 6. Cross section of a coronary artery with an atherosclerotic lesion.