Stereotactic
Image Guidance in Brain Surgery
Gamma Knife®
In many cases, invasive
neurosurgery is not an option, because a tumor or other abnormality is
located deep within the brain, surrounded by other delicate critical
areas.
Radiosurgery is an enabling technology that can
treat tumors which may have been otherwise termed inoperable. Radiosurgery
allows a neurosurgeon to operate on the brain without a scalpel and
without opening the skull, thus direct visualization is not possible,
and localization of surgical area completely relies on image
guidance. In radiative treatment, an array of radiation beams,
converging from many different directions, can be focused on the target with a fraction of a millimeter precision.

Gamma Knife was originally developed
by Swedish neurosurgeon Lars Leksell in 1967, and is currently
commercialized by Swedish company Elekta. Gamma Knife technology combines
images from stereotactic CT, MRI, positron emission
tomography (PET), magnetoencephalography (MEG), and/or cerebral
angiography, and uses them for target determination and radiation beam
focusing. Gamma Knife is primarily targeted for brain tumors (both benign and malignant), but is also used in treatment of arteriovenous malformations, trigeminal neuralgia, acoustic neuromas, and pituitary tumors.
Gamma Knife system consists of the following major components:
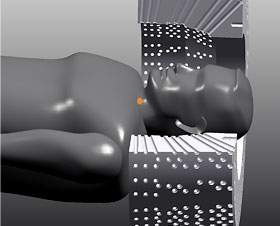
- Radiation unit that contains more than 200 cobalt-60 sources of gamma
radiation, placed in a circular array of a heavily shielded assembly;
- Beam-focusing unit with tungsten collimators,
which focuses radiation beams at multiple target points in a highly
conformal way, minimizing the risk of damage to brain tissue outside of
targets;
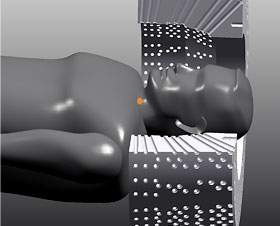
- Patient couch with electric bed system and precise robotic motion control, which positions the patient’s head at the focus point with accuracy of less than 0.3 millimeter;
- Control console and planning computer system, which analyzes
preoperative imaging data and performs the stereotactic guidance and
planning of beam trajectories.
What future directions and challenges may be pursued by biomedical engineering with respect to this technology?
- The system could be integrated with intraoperative imaging systems.
- With current systems, the patient is required to wear a specialized
helmet that is surgically fixed to the skull in order to eliminate any
motion of the focal area. Future systems could track motion in
real-time and compensate for it with adaptive beam forming.