| Image Guided Surgical Robots | |||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||
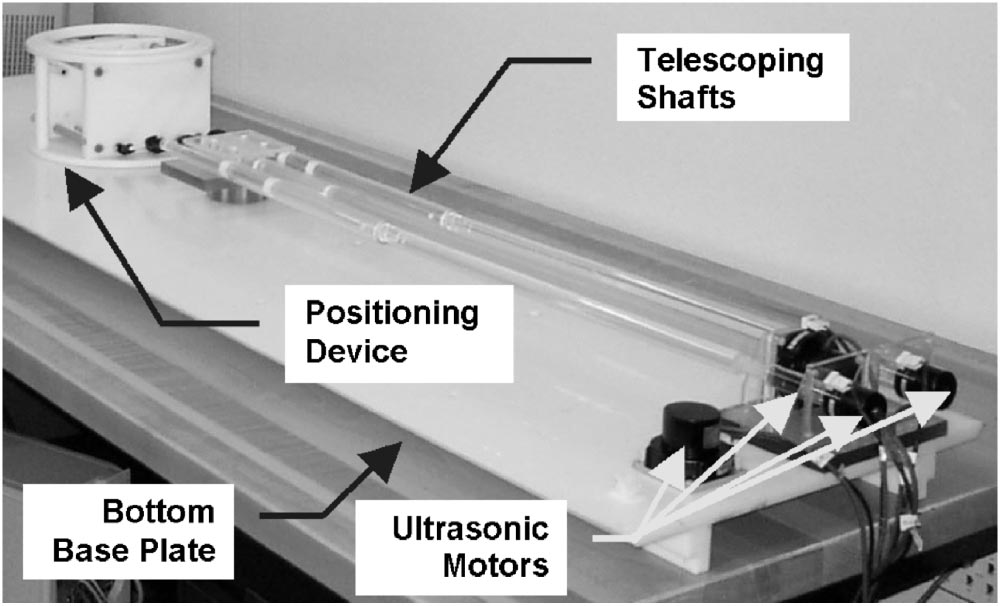
MRI guided surgical robotsAlthough its high resolution, relative safety, and non-invasive nature make MRI an attractive modality for image guided robotics, there are a number of challenges impeding the design of MR guided robots. Not only do the RF pulses used for tissue excitation make the use of unshielded electronics all but impossible, but the large magnetic field precludes the use of both ferrous metal components and electromagnetic actuators. Even the use of non-ferrous metals is deemed undesirable due to their tendency to create large scanning artifacts. Despite these challenges, there are a number of groups that have developed successful MR compatible robots. One of the earliest MR guided robots was described by Chinzei et al (2000). To simplify some of the MR compatibility issues discussed above, the chinzei et al. group designed their robot to be compatible with an interoperative MRI system (see figure1). However, even outside of the bore, the close proximity of the electric field forced the group to use piezo electric motors to control their device.
The device described by Chinzei et al. consisted of two piezoelectrically driven manipulators with a total of five degrees of freedom (x,y,and z on one arm and x and y on the other). By controlling two points in space with a total of five degrees of freedom, the device was able to control the precise position of a catheter, needle, or other surgical tool. As such, the device had the potential to enable minimally invasive biopsies, needle surgeries, or radioactive seed placement procedures. The piezoelectric motors were located outside of the MRI bore. Although this improved the SNR of the MRI scanner and simplified the control of the actuators, it also reduced the precision with which the actuators could control their end effector. As such, the device was not suitable for fully automated procedures, but was rather intended to assist surgeons in minimally invasive procedures. Moreover, since the robot could not be placed within the MRI bore itself, the position of the robot could not be directly registered to the position of the patient using MR data. The fact that the scanner and the robot had separate workspaces made it very difficult to accurately determine the position of the robots end effector with respect to the patient. Although the Chinzei et al device left much to be desired, it demonstrated that it demonstrated that MR compatible surgical robotic systems were indeed possible. As such, it should come as no surprise that a number of comparable devices were developed in response. For a brief summary of some of these devices see figure 2.
Perhaps the most impressive MR compatible surgical robot to date is the device described by patriciu et al (2007) (figure 3 and video 1). Unlike the majority of its predecessors, which used piezoelectric actuators, the patriciu et al device used custom built pneumatic stepper motors to provide precise, MR compatible actuation. To date, the patriciu et al device appears to be the only MR compatible robot capable of performing a fully automated needle surgery. Because the device is composed entirely of ceramics, plastics, and other fully MR compatible materials, the device is able to operate freely within the MR bore. Since the robot and the scanner share the same workspace, it is possible to register the position of the robot directly with the position of the objects being scanned. to fully define the position of the robot in MR space, small MR opaque markers are placed near the end effector of the robot. Not only does registering the robot in this way greatly increase the accuracy of the device, but it allows for the possibility of fully automated MR guidance. References
|