| Cataract Surgery and Intraocular Lens Technology |
Posterior Capsular Opacfication and its Cause
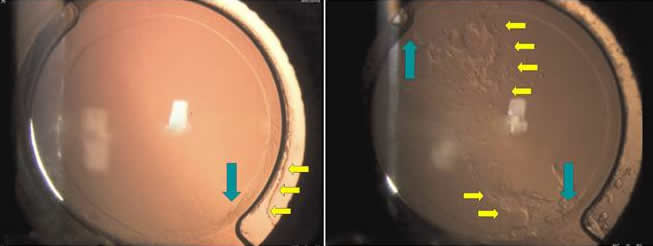
Figure 1. 1-year postoperative lens implantation shows almost no sign of posterior opacification. (left) The same lens was imaged 2-year postoperative, showing regenerating cortex migration past the board optic-haptic junction and onto the posterior capsule. The arrows indicate the start of cell migration onto the lens (left) and areas characterized with prominent cellular deposits (right). (Dewey)
The most common post-operative complication proceeding cataract surgery is secondary cataract formation or posterior opacification (PCO). After IOL implantation, an induced immune response within the capsular is undesirable but also unavoidable for the most part. It is well documented that some extent of foreign body reaction occurs in all eyes following IOL implantation; (Figure 1) an invasive procedure which involves phacoemulsification, capsulorhexis and lens placement. In specific, the cellular response that occurs after IOL implantation is a result of 1.) the breakdown of the blood-aqueous barrier and 2.) foreign body reaction induced by the lens material. (Boer) Breakdown of the blood-aqueous barrier is followed by an increase in protein and cellular content of the anterior chamber which can lead to postoperative complications such as anterior capsule opacification. The presence of an inflammatory response or foreign body reaction is defined by cellular deposits of migrated lens epithelial cells, macrophages, leukocytes and giant cells induced by respective chemotactic factors on the surface of intraocular lenses. (Boer) Further complications can occur when epithelial-mesenchymal transition-related fibrosis and lentricular fiber regeneration (formation of Sommerring’s ring and Elschnig’s pearl) form on the surface of implants. (Saika)
Nd:YAG posterior capsulotomy
Though PCO is unavoidable to a certain extent, it may not necessarily affect one's vision, depending on the severity of the case. In the case of minor PCO, most patients will not observe any decrease in vision or clarity. But in 40-50% of PCO cases, vision will diminish with the advancement of the secondary cataract. In these cases, a patient may choose to undergo a laser surgery called Nd:YAG posterior capsulotomy to correct this problem.

Figure 2. A typical Nd:YAG configuration
A laser (Nd:YAG laser) is used to cut a hole in the clouded back lining of the IOL to allow light to pass through the membrane to the retina at the back of the eye (Figure 2). The Nd:YAG laser is currently considered the best way to remove the back lining of the lens capsule but repeat procedures and costs are undesirable. Other treatment and prevent measures are currently being research as discussed here.
References:
de Boer, J.H.; Hack, C.E.; Verhoeven, A.J.; Baarsma, G.S.; de Jong, P.T.; Rademakers, A.J.; de Vries-Knoppert, W.A.; Rothova, A. & Kijlstra, A. (1993), 'Chemoattractant and neutrophil degranulation activities related to interleukin-8 in vitreous fluid in uveitis and vitreoretinal disorders.', Invest Ophthalmol Vis Sci 34(12), 3376--3385.
Dewey, S. (2006), 'Posterior capsule opacification.', Curr Opin Ophthalmol 17(1), 45--53.
Saika, S. (2004), 'Relationship between posterior capsule opacification and intraocular lens biocompatibility.', Prog Retin Eye Res 23(3), 283--305.
All Right Reserved © 2007 by H Sin