Background
Problem
Over 400 million people in the world are afflicted with bladder disease. 1 The end result of these diseases sometimes requires a cystectomy (resection of the bladder) which calls for a replacement of the entire organ or to partially repair the damaged areas. Many of the issues that complicate transplants also affect bladder replacements. There are not enough donors, there are immunological responses, or the replacement is not exactly the same tissue. In the case of bladders, the gold standard for the replacement of bladders is to resect a piece of stomach or bowel from the same patient to replace the lost tissue. This requires additional surgery which increases the chances of infection and complications. Another problem with replacing the tissue was the difference in tissue characteristics between the replacement and the original. 1-4 Bowel tissue is different from bladder tissue in many ways which range from mechanical properties such as the elasticity of the tissue to the flow nutrients and waste across the tissue layers.1 In the case of the bladder, the permeability characteristics of the tissue cannot be replaced easily with just bowel or stomach tissues.1-3 Thus, researchers and scientists sought for the ideal replacement of bladder tissue.
Requirements for Bladder Replacement or Repair
An ideal bladder replacement would be able to:
- 1) Emulate the mechanical and elastic properties of the bladder
- 2) Have the same permeability and membrane characteristics of the bladder.
- 3) Not illicit any immune or adverse reactions in the host organism.
This would be accomplished by a group under Dr. Anthony Atala at Wake Forest.3 They were the first group to grow autologous bladder tissue and transplant them into human patients in April of 2006. They were able to recreate the bladder using a combination of using the patient's cells and reconstructing the bladder using tissue engineering techniques. To understand their accomplishment we must first understand the anatomy of the bladder.
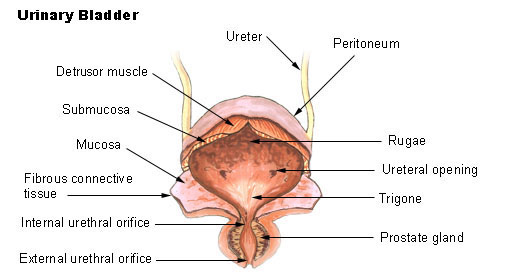
Figure 1: Anatomy of the bladder, courtesy of http://training.seer.cancer.gov/module_anatomy/images/illu_bladder.jpg
Bladder anatomy
The bladder is a hollow organ which is designed to hold up to 1.1-1.3L of fluids. 3 As shown below in figure 1, we are able to notice that the bladder has different layers ranging from the mucosa to the submucosa, along with the detrusor muscle. The bladder is able to stretch up to 15 times its original size. The bladder is connected to the kidneys via the ureter and collects the urine waste as a reservoir. The bladder is extremely elastic and can grow to accommodate the collection of urine. A range of diseases can disrupt this function. Usually the bladder is not resected unless prior therapies are deemed unable to help. Diseases ranging from genetic to metabolic can affect the bladder as well as cancer and trauma.
Diseases of the bladder
Diseases ranging from cogenital defects such as bladder exstrophy, myelomeningocele, and defective urethral valves to bladder cancer may require cystoplasty to repair the damaged bladder tissue.1,5 Over an estimated 400 million patients suffer from end stage bladder disease and when drug therapies fail, a cystectomy is performed to remove the entire organ or part of it. In order to restore mechanical and physiological properties of the bladder, researchers turned to the realm of tissue engineering to aid in the reconstruction of the bladder.
Click here to learn about Tissue Engineering
