
The Future of Peripheral Axonal Nerve Guide Technology:
With the clinical success of multiple types of resorbable and non-resorbable nerve guide technologies, continued research seeks to consistently bridge longer nerve gaps with higher average success rates. The concept of Critical Length (LC) has been proposed to cross compare the effectiveness of different nerve guides. LC is defined as the inflection point in the comparison chart of bridged gap length versus the number of successful nerve regeneration animals[19]. For primates LC is significantly greater than rodents at approximately 30mm[19].
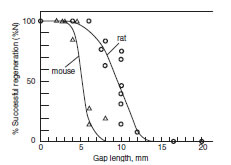
Researchers Zhang and Yannas proposed a metric known as Critical Length LC to cross compare the effectiveness of nerve guides as a function of distance versus the percentage of successful reinnervations for a particular study animal and technique (Image care of Zhang and Yannas, 2005)
The inclusion of guide matrices within the lumen of nerve guide typically increases the critical length of that particular device[20]. Commonly viscoelastic hydrogels with a high water content work well, such as loosely wound collagen or Matrigel[20]. The immunogenic nature of Matrigel, derived from mouse sarcoma tissue, limits the use of this material to research only. Fibrin formed with peptide sequence incorporated from laminin has shown promise as a clinically applicable filler material [21].
Continued research has led to the exploration of aligned matrices as compared to the isotropic matrices previously discussed. For a rat model, an empty silicone nerve guide has a determined LC value of 9.7mm, yet with the introduction of a Collagen-GAG matrix, the LC value increases to 14.8mm[20]. In increase in the LC value of 4.7mm can be observed with aligned fibrin matrices[20].
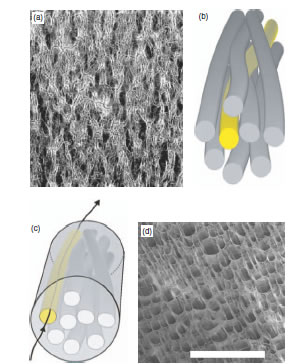
Some approaches for oriented scaffolds/matrices for peripheral nerve guide technology. Magnetic alignment has shown improvement of LC values for collagen, fibrin, and Matrigel matrices (a). Both fibers (b) and channels (c) demonstrate guidance properties, while uniaxial freezing methods for Polyethylene Glycol (PEG) scaffold formation results in many oriented channels (d). (Image care of Van Blitterswijk's Tissue Engineering)
Success has been demonstrated using nerve guides consisting of formalin fixed human amniotic membrane augmented with added neurotrophic factors and Haluronic Acid (HA) in the core of the guide. The effects of HA indicate a 45% better axonal regeneration, as assessed by histological observation, than when HA was omitted in the control. According to the study, the early presence of the HA matrix favors the migration of macrophages into the injured tissue to allow proper degradation in preparation for regeneration. The degradation products of HA moderate the inflammatory response and stimulate angiogenesis, leading to proper profusion. This may promote nerve healing via regeneration rather than scarring[22]. Continued work is necessary to improve the imounogenesis of the formalin fixed tissue.
Recently studies of exotic materials have been attempted to tailor the resorbable properties of matricees. Notably silk and spider silk. Both materials offer the ability to be treated such that neural cells attach to their surfaces [23]. Continued work is necessary to determine necessary degradation rates and construction parameters to take these models into en vivo experiments.
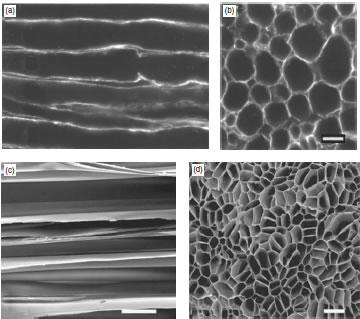
Shown on top (a), (b) are length and cross sections of natural lamina tubes present in the distal nerve component after Wallerian degradation. (Scale bar=200 micron) Below (c), (d) are scaffolds formed by uniaxial freezing of PEG. Note the similarities in shape and scale. (Image care of Van Blitterswijk's Tissue Engineering)
As demonstrated with experimental collagen matrices, the use of neurotrophic growth factors has shown to affect the regeneration of neurons. After an injury, the space within a nerve guide fills up with cytokines released from the distal stump. TrkA, TrkB, TrkC, Glial Derived Neurotrophic Factor(GDNF), Cilliary Neurotrophic Factor (CNTF), and Brain Derived Neurotrophic Factor (BDNF) assist in the maintenance and regrowth of proximal neurites[20]. Specifically CNTF and BDNF when applied via a pump to the site of the injury improved functional recovery after an end-to-end repair. [20] Continued multi- parameter studies are necessary to determine the role of these factors when used in resorbable or simply filled lumen nerve guides.
Conclusion:
Peripheral axonal nerve guide technology has progressed from a study in curiosity where any seemingly reasonable material was tried in hope of reinnervation success to a methodical study of the application of material science and biomedical engineering. The next generation of peripheral nerve guides will undoubtedly utilize neurotrophic, material alignment, and resorbable technologies. Within each individual field a plethora of research questions and problems still exist. With continued en vitro, en vivo, and clinical studies larger gaps will be bridged with a higher reinnervation success rate.
|