| Deep Brain Stimlation for Treatment of Severe Mental Disorders |  |
| Navigation: | What is Deep Brain Stimulation? | |
Home What is DBS? Technology Advances Mental Disorder Treatment Future Work References |
Origin and History of DBS |
|
After being approved in July of 1997 by the FDA in the United States for use in patients with essential temors, the number of Deep Brian Stimulators has grown steadily. Currently, there are over 3,000 DBSs being implanted annually, mainly for essential tremors, Parkinson's Disiese, and dystonia. With advances in imaging, robotics, power sources, and mechanism understanding, DBS is venturing into the field of Mental Disorders. Untreatable cases of major mental depression and obcessive-compulsive disorder are now under investigation for treatment with DBS. There is a greater level of insight that must be granted toward these cases due to the lack of instantaneous feedback that is present in movement disorder.
|
||
Components of DBS |
||
|
Implantable stimulators consist of three pieces that are all contained inside the body. The main body that controls the pulsing and the power is called the Neurostimulator. It is the pacemaker of the device and generates the electrical impulses that are sent to the brain through the leads.
The leads that run from the neurostimulator to the electrodes consists of four to eight insulated wires. These wires are housed in polyurethane to provide insulation from the surrounding tissue.
A single probes contains all four of the electrodes. The elctrodes are manufactured out of a platinum/iridium blend. This contact pad is the location of the current output. |
|
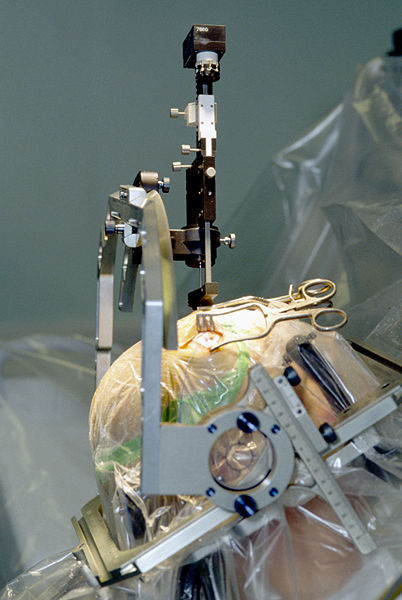
Procedure for implantation |
||
|
|
|
| <--Return to Home | |
| University of California, Irvine |