Why is Monitoring Hematocrit Important?
There are two main reasons for monitoring Hematocrit, to aid in diagnosis and to ensure effective life support in the operating/emergency room.
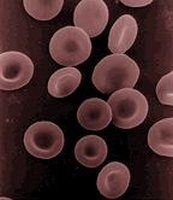
There are many diseases that can be detected by testing Hematocrit. Anemia, a condition of low red blood cell count, is the most common blood disorder. There are also diseases of increased red blood cells, Polycythemias, which increase the viscosity of the blood and can cause a wide variety of symptoms.
Abnormal Hematocrit may also indicate illness. For example, chronic obstructive pulmonary disease can cause an increase in the production of red blood cells while a low red blood cell count could be an indication of a hemorrhage or ectopic pregnancy. (www.wikipedia.org)
During critical care, a patient's hematocrit may fluctuate drastically. Shock, severe burns, dehydration, severe diarrhea, can all lower the water content of the body and consequently the plasma levels in the blood. This decrease in plasma causes an increase in Hematocrit, the ratio of red blood cells to volume in the blood. High Hematocrit levels in an emergency setting are treated with the administration of plasma which restores the red blood cell to volume ratio of the blood.
Loss of blood due to injury or surgery will cause a drop in hematocrit. This must be acted upon immediately to preserve the patient's life. Transfusions are given to maintain at least a minimal Hematocrit of 21%. Each unit of red blood cells restores approximately 3% - 4% Hematocrit in an adult patient. One of the key challenges during surgery is the maintenance of adequate Hematocrit because of the patient's loss of blood during the procedure. Adequate levels must be maintained while not deviating from the norm in either direction. (health.enotes.com/surgery-encyclopedia/hematocrit)
