Introduction to Optical Detection
Over the years, many approaches have been taken in the attempt to measure blood glucose levels more accurately, less invasively and continuously. In 1993, Quan et al investigated non-invasive infrared photoacoustic detection of blood glucose. The goal was to develop a non-invasive system to monitor blood glucose levels. Prior to their work, many had investigated into optical transmission and spectroscopic techniques. Using a gelatin based in vivo model they demonstrated that the optical absorption due to glucose is small compared to photoacoustic detection. Additionally, the linear relationship between the photoacoustic response and glucose levels suggests this system could effectively and non-invasively monitor blood glucose levels.
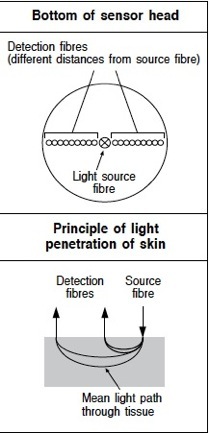
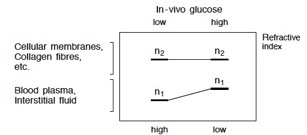
In 1998, Heinemann et al sought to improve insulin therapy using light absorption and light scattering techniques. One problem was that glucose independent variations of the scattering coefficient of the skin makes this system less reliable. This problem is partially solved by modifying the sensor geometry and algorithms for the scattering coefficient. This method proved more accurate than spectrophotometry, making it a possible solution for the continuous measurement of blood glucose levels non-invasively.
The following year, Garg et al compared glucose measurements taken via iontophpretic extraction from a GlucoseWatch to standard blood glucose measurements. They found that GlucoWatch values correlated well with values found using an analyzer in a clinical setting. They found that increasing the frequency of glucose readings could improve glucose regulation and prevent severe hypoglycemia. Later that year, Gabriely et al created a transcutaneous near-infrared spectroscopy system for non-invasive blood glucose monitoring. It is well known that maintaining near-euglycemia in patients with type-1 diabetes can delay long term problems. To attain glucose levels within a narrow range frequent measurements must be taken. They found that their transcutaneous system produced measurements that correlated closely with the predicted venous glucose levels in the hypoglycemic range. Additionally, this system showed increased sensitivity when compared to previous optical glucose techniques.