EEG and MRI Techniques for Diagnosing Epilepsy:
Prior to the ECoG resection surgery, the electrode grids are mapped onto the patient through the use of magnetic resonance imaging (MRI) and electroencephalography (EEG), as shown in the simulate MRI image in Figure 4. The surgeon then begins the procedure by performing a craniotomy and exposing the region of interest identified by other imaging techniques. A grid(s) of electrodes are then placed onto the desired region predetermined by MRI and EEG analyses.
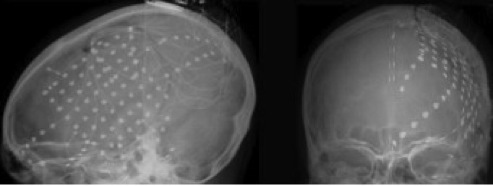
Figure 4: Spatial Electrode Arrangement Using MRI Imaging Techniques (7)
The following video will also give insight in how MRI and EEG techniques are used to diagnose epilepsy and the need for resection surgery and ECoG mapping of epileptogenic lesions:
Surgical Approaches for Resection Surgery Using ECoG:
In order to use ECoG to record neural activity and localize epileptogenic zones, a craniometry must be done by the surgeon in order to go past the skull and allow subdural placement of an electrode. This is of course done after epidural placement, i.e. after using EEG techniques to further localize the epileptogenic zone. The following link shows a video of a resection surgery using ECoG to treat epilepsy:
Google Video of a Resection Surgery Using ECoG to Treat Epilepsy
Besides using ECoG as a technique to define the epileptogenic zone for resection surgery, there are many other intraoperative mapping techniques that can be used. The following video gives further insight into other operative techniques for epilepsy surgery as well as an overview of different operative types of surgery to treat epilepsy:
ECoG Approaches for Defining Epileptogenic Zones:
Once an ECoG array is implanted into the patient after a craniometry, the surgeon will then stimulate various regions of the brain by using a set of separate and mobile stimulating electrodes. The resultant evoked responses are recorded by the electrode grid in order to localize the epileptogenic region. This is usually done during the surgery, although current ECoG array implants can be implanted for several weeks for better monitoring and definition of epileptogenic boundaries and zones, as the success of the surgery is highly dependent upon the localization of the zone.
The following figure shows the distribution of inter-ictal discharges recorded from the implanted subdural electrodes in the left anterior lateral region. Also shown in the figure is a brain cartoon that shows the corresponding regions inside the circle and regions of ECoG recordings (8).

Figure 5: Real Time ECoG Recordings from Subdural Electrodes
After monitoring the ECoG recordings for up to several weeks, the neurosurgeons can then perform a resection surgery. The following video will give insight into the use of ECoG to perform a resection surgery as well as other techniques (such as EEG and WADA) used during the assessment of the epileptogenic zone:
Advantages and Disadvantages of Using ECoG:
Like EEG techniques used prior to surgery, there are many advantages and disadvantages to ECoG surgery for defining epileptogenic zones. Below are a few of the advantages for using extraoperative and intraoperative ECoG techniques to define epileptogenic zones:
-
(1) They offer flexible placement of recording and stimulation electrodes
-
(2) Recordings can be performed before and after each stage of resection to assess the presence/absence of epileptic activity
-
(3) It allows direct electrical stimulation of the brain so that the regions involved in functions that must be spared by resection can be avoided with a high degree of confidence (9)
-
(4) They offer high spatial resolution (0.5-3 mm)
-
(5) There is excellent temporal resolution (5 ms)
-
(6) ECoG signals have a better signal to noise ratio (SNR) than scalp EEG
-
(7) It allows recording and/or stimulation of actual neural activity
-
(8) ECoG allows for real-time interaction with the patient
Unfortunately, there are still a few disadvantages for using ECoG techniques as a presurgical technique for resection surgery. The following are just a few disadvantages of using ECoG to define epileptogenic zones:
-
(1) There is limited sampling time
-
(2) Spontaneous epileptic activity consists exclusively of inter-ictal spikes and sharp waves, and thus seizures are rarely recorded
-
(3) It is impossible to distinguish primary epileptic discharges from secondary propagated discharges that arise at a distant epileptogenic site
-
(4)Both background activity and epileptic discharges may be altered by aneasthetics, narcotic analgesic, and by the surgery itself
-
(5) It is very invasive, and researchers must cooperate with epilepsy patients and neurosurgeons to determine the requirement of this invasive procedure
-
(6) There is a limited view of the brain during surgery
-
(7) There is a limited duration of the surgery; thus, if you’re looking for seizure activity during an intraoperative procedure, you may not see any.
Even though there are a few disadvantages to using ECoG for resection surgery, it is still considered the “gold standard” for assessing epileptogenic zones. EEG techniques do not offer the same amount of spatial resolution to define the proper epileptogenic zone without causing too much cognitive and neuronal damage, which is why EEG techniques can only be used as an initial assessment of the epileptogenic zone. The following videos discusses more of the benefits for epilepsy surgery as a whole, and should be considered alongside the benefits of using ECoG when approaching epilepsy surgery:
In order to overcome the disadvantages of epilepsy surgery as well as the disadvantages of using ECoG over other mapping techniques, we must consider the design criteria of ECoG to properly determine the future approaches for resection surgery using ECoG. The design criteria section of this website will discuss the limitations and criteria for ECoG design and use in resection surgery for epilepsy treatment.