

|
Deep Brain Stimulation and Applications |
|
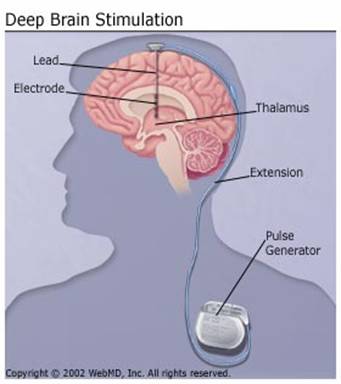
Introduction: Deep Brain Stimulation is a procedure that involves the use of small electrodes to transmit electrical impulses to specific parts of the brain. It is primarily used to treat patients suffering from Parkinsonís disease and Multiple Sclerosis but can also be applied to several other neurodegenerative conditions. It is a reversible procedure based on implantation of miniature electrodes in the targeted brain areas to generate electric impulses. The DBS system consists of three components: 1. The lead/electrode is a thin, insulated wire, inserted through a small opening in the skull and implanted in the brain. The tip of the electrode is positioned within the targeted brain area. 2. The extension is an insulated wire that is passed under the skin of the head, neck, and shoulder, connectng the lead to the neurostimulator. 3. The neurostimulator/ battery pack is implanted under the skin near the collarbone. In some cases it may be implanted lower in the chest or under the skin over the abdomen. Procedure: The area of the brain to implant the electrodes is recognized using imaging techniques such as MRI(Magnetic Resonance Imaging) or using a CT (Coherence Tomography) scan. These electrodes are of the order of approximately 1mm and are capable of generating steady electrical impulses. These electrodes have to be surgically implanted in the desired section of the brain based on the disease and its symptoms, which is either one side of the brain or both. Most patients with Parkinsonís disease require the electrode implantation on both sides of the brain. The working principle of these electrodes is very similar to that of a pacemaker. An electrode recoding technique map can be used to target the specific areas that need to be reached by electric stimuli. †††††††††††††††† †††††††††††††††† Upon identification of the implant location which is mainly the thalamus in the case of Parkinsonís disease, the permanent electrodes are implanted. The loose ends are placed underneath the skin of the head and the incision is closed with sutures. One week later, the patient is readmitted to the hospital for a very brief time. The patient is placed under general anesthesia and the extension wires are disconnected from the loose ends of the electrodes and then connected to the impulse generators that are usually implanted in the chest area. Two to four weeks later, the impulse generator is turned on and adjusted to yield the desired output. It usually takes a few weeks until the simulators and medications are adjusted sufficiently for patients to receive adequate symptom relief. When switched on, the generator delivers continuous low-voltage electrical pulses to the brain, which apparently block the abnormal firing of neurons ó caused in Parkinson's by a lack of dopamine. DBS on the average is capable of reducing 50% to 60% of the symptoms that characterize Parkinson's disease, including tremors, stiffness, slowness, gait problems and uncontrollable writhing, allowing patientís extraordinary gains in movement and control. Statistics: More than 35,000 patients around the world have had DBS electrodes implanted in their brains, and there are 250 centers in the U.S. that perform the procedure. The treatment of neurodegenerative disorders using DBS is mainly performed in patients with relatively advanced cases of the disease and those for whom medication alone is inadequate. |