1) Glucose Sensor
2) Insulin pump
3) A set of algorithms that relate the glucose
sensor to the insulin pump
Having all three of these elements in a long-term implantable device
is considered to be a "closed-loop" system, the
holy grail of battling Type 1 diabetes. The insulin pumping
mechanism has been well worked-out and is not really considered a "challenge".
In fact, implanted insulin pumps
currently can last up to five years. The following is an external
link comparing the currently available external insulin pumps on the
market in the U.S.
Comparison of Insulin Pumps
The real problem lies in determining the
set of algorithms that synchronizes the glucose sensor with the
insulin pump as well as creating an implantable continuous glucose sensor. It
is well agreed upon that there is not a linear relationship between
the glucose concentrations and the amount of insulin that Beta cells
release. There
is a whole field of research dedicated to determining the algorithms
and they will without a doubt improve with time.
Achieving a continuous implanted glucose sensor is another feat of
its own. There are currently no available long-term implantable
continuous glucose sensors. Currently the longest life span of an
FDA approved subcutaneous implantable glucose sensor is at 2 weeks
and one is produced by DexCom (www.DexCom.com)
and another MiniMed Medtronic (www.MiniMed.com).
Because these subcutaneous implantable glucose sensors are based on
the enzyme glucose-oxidase their lifespan is currently limited to
around two weeks, after which the enzyme has been degraded too much
to be considered accurate. In addition, these sensors are no where
near ideal. They must be calibrated 4-6
times a day by the patient taking an "old fashioned" blood prick.
Moreover, these are subcutaneous glucose sensors and, thus, they are
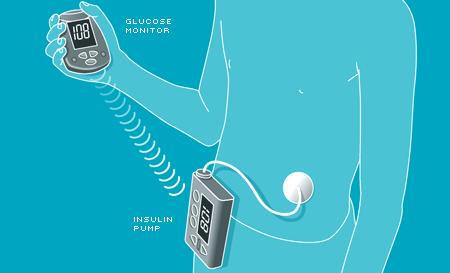
not truly a fully implantable sensor. Currently the
MiniMed
Paradigm REAL-Time System is the only commercially available
system that integrates an insulin pump with real time continuous
glucose monitor. The following is a diagram of the MiniMed's
Paradigm REAL-Time system:
Conclusion: Currently the most common
commercial approach to this problem. While the development of an
insulin pump is considered a completed task, we are still far from
having a long-term implantable glucose sensor, and having a set of
algorithms that fully relate the insulin pump to the glucose sensor.
Optimizing this approach might be the most commercially successful
approach.
Next Section:
Design Criteria