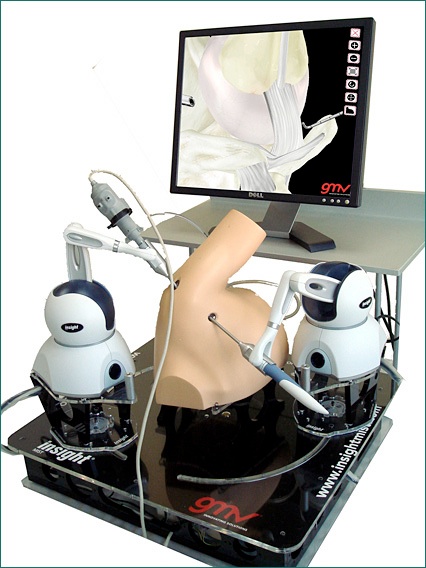
Surgical simulation through haptic technology
Advanced technology is allowing computers to power far more realistic, guided learning experiences than on static "dummies," which will directly benefit clinicians and patients while still delivering key benefits of simulation, including the ability to avoid the use of cadavers, animals, and live-patient learning.
Haptic medical simulations provide force feedback and are based on sophisticated, high-fidelity haptic devices and software that deliver greater precision, differentiation between materials such as bone and soft tissue, and a more realistic sense of touch.
The haptics most frequently seen in medical simulation and training uses technology known as proprioceptive "force feedback," where users hold a tool or stylus that pushes back on the user's hand when it makes contact with virtual objects. The stylus is usually powered by a motor, or in a recent case, by magnetic levitation forces, and programmed by software to deliver specific levels of force or "feeling." Such forces can be programmed to simulate the sensation of interacting with different organs by knowing the material properties of tissue, muscle, fat, open cavities, or more specific anatomical substructures.


Traditional practice for teaching procedures to surgical residents is to "see one, do one, teach one" via clinician supervision with expensive bone specimens from cadavers or on real patients. Neither option facilitates thorough, risk-free training. Cadavers are costly and usually in short supply, with some countries (for example, the United Kingdom) banning them altogether. Patient-based learning — even under the highly supervised hospital settings of today's medical centers — interjects an element of risk and malpractice concerns, particularly with high-risk procedures such as temporal bone drilling near the brain, where the slightest deviation can create widespread and permanent adverse consequences.
There are several opportunities for computer-based, haptically-enabled training simulators to beneficially impact medical education: guided lessons without the need for a real mentor present, simulating real patient anatomy and functions and the relevant anatomic variants, and automatic or batched assessment by the teacher. Medical students can practice a procedure repeatedly — an unlimited number of times — until they learn to "feel" how a procedure is done, and be skill-tested in a controlled, measurable environment.