The delivery of radiation to rapidly differentiating tumoral cells is the main aim in the therapy. It is necessary, on the other hand, to value the limiting factor to the quantity of radiation dose delivered, that consists in the presence of healthy tissues surrounding the tumor and that can be damaged. Avoiding collateral damage coming from radiation induced toxicity is also an important point in the therapy. Some considerations need to be done in order to understand the importance and innovation of Image Guided Radiation Therapies.
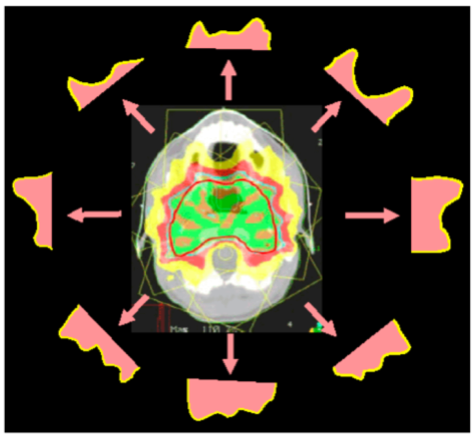
First of all, radiation is produced through linear accelerators, it can have different Linear Energy Transfer (LET) to tissue depending on attenuation and energy of the beam. These factors need to be taken into careful consideration when preparing the Therapy Plan. Traditionally an MRI scan of the patient is used and in each slice the tumor is marked. On various software programs the 3D image is composed and the plan is prepared. The irradiated volume encompasses the gross tumor volume (GTV) and a margin is added to assure a proper coverage of the clinical target volume (CTV), the resulting volume is called planning target volume (PTV). This compensates for daily positioning errors and internal motion of organs and is the final volume to which radiation dose is prescribed.
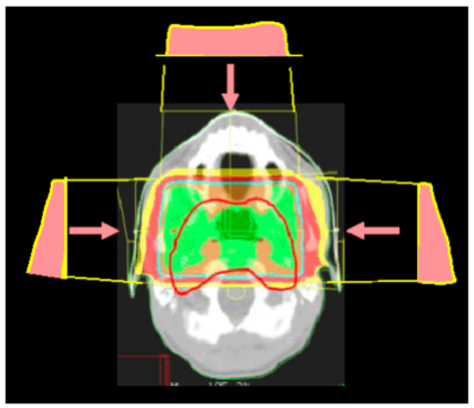
During the planning, if possible, organs at risk (OAR) are taken into consideration. OAR are organs that are close or in line with PTV. Any damage at them could cause a loss of functionality in the patient.
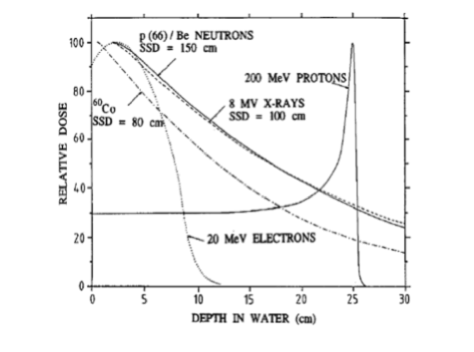
As it is shown in the above graph, radiation deposits dose along the depth with a specific function. The total dose on a single point is given by the sum of the doses deposited from each beam used. Traditionally the number of beams used is 3, 2 lateral and one frontal. Along time the technique has been improved, using more beams. In fact with a higher number of beams the dose can be distributed more precisely thus reducing the collateral damage to healthy tissues. So techniques with 6 beams were developed, and lastly Intensity Modulated Radiation Therapy (IMRT) that makes use of a high number of beams (more than 20) from an optimization via software program.
Another relevant point is patient positioning. In order to achieve precision the patient must be hold in the same position in the different planning days. This is done by conforming holders on the patient’s shape and performing portal imaging prior to each session with bone reference to evaluate the variation in position of the patient. If the position differs more than a specific value (usually 5mm) the patient is repositioned.
